Smoking and the risk of contracting SARS-CoV-2 and COVID-19 Coronavirus Disease COVID Tobacco Smoking LancetRespirMed UCSF RoswellPark Stanford Yale USC VUMChealth uofl
By Nidhi Saha, BDSAug 21 2022Reviewed by Benedette Cuffari, M.Sc. Smoking increases the risk of respiratory infections, such as colds, flu, pneumonia, and tuberculosis. Smoking may also contribute to coronavirus disease 2019 complications.
More specifically, these substances appear to directly damage the epithelial cells, which subsequently impacts the epithelial barrier and mucociliary clearance. In addition to these direct effects, these damaged cells release modified molecules into the lungs, which stimulate specific receptors that ultimately activate innate and acquired immune responses.
The researchers analyzed the behavioral mechanisms associated with tobacco consumption on COVID-19 and inflammatory immune responses. Furthermore, they also screened risk factors for the development of public health policies and patient care delivery. Study findings Epidemiological studies investigating the impact of cigarette smoking on SARS-CoV-2 infection have rendered mixed results. Thus, further research is needed to ascertain whether smoking or the use of other tobacco products contributes to the susceptibility to COVID-19.
Tobacco products contain a wide range of potentially toxic chemicals, while several harmful chemicals are also formed during the aerosolization process due to the heating or combustion of the product. The use of tobacco products can result in substantial damage; however, it remains unclear how individual chemicals and constituents contribute to these pathophysiological effects.
United Kingdom Latest News, United Kingdom Headlines
Similar News:You can also read news stories similar to this one that we have collected from other news sources.
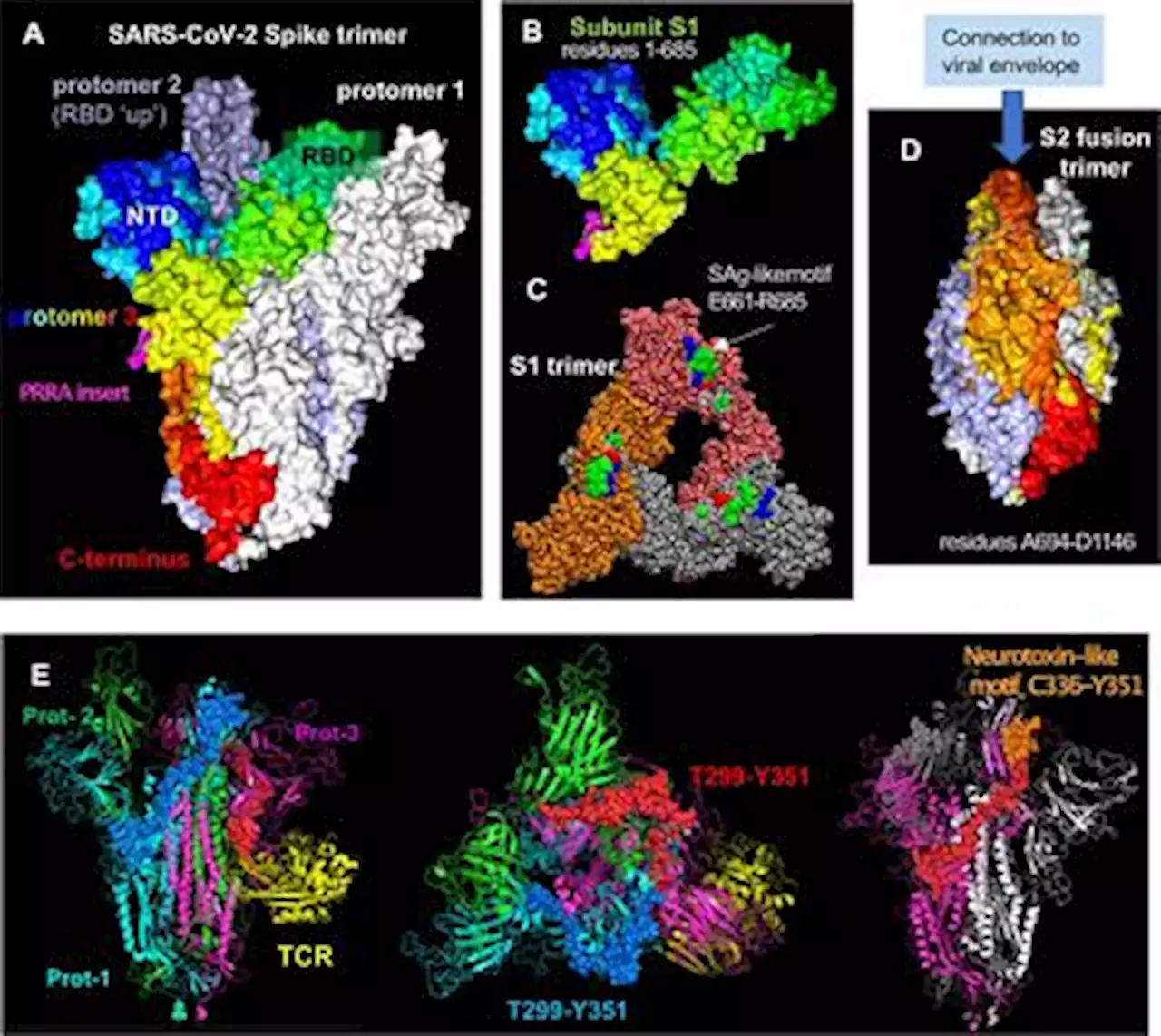 Frontiers | Multisystem Inflammatory Syndrome in Children and Long COVID: The SARS-CoV-2 Viral Superantigen HypothesisMultisystem inflammatory syndrome in children (MIS-C) is a febrile pediatric inflammatory disease that may develop weeks after initial SARS-CoV-2 infection or exposure. MIS-C involves systemic hyperinflammation and multiorgan involvement, including severe cardiovascular, gastrointestinal (GI) and neurological symptoms. Some clinical attributes of MIS-C—such as persistent fever, rashes, conjunctivitis and oral mucosa changes (red fissured lips and strawberry tongue)—overlap with features of Kawasaki disease (KD). In addition, MIS-C shares striking clinical similarities with toxic shock syndrome (TSS), which is triggered by bacterial superantigens (SAgs). The remarkable similarities between MIS-C and TSS prompted a search for SAg-like structures in the SARS-CoV-2 virus and the discovery of a unique SAg-like motif highly similar to a Staphylococcal enterotoxin B (SEB) fragment in the SARS-CoV-2 spike 1 (S1) glycoprotein. Computational studies suggest that the SAg-like motif has a high affinity for binding T-cell receptors (TCRs) and MHC Class II proteins. Immunosequencing of peripheral blood samples from MIS-C patients revealed a profound expansion of TCR β variable gene 11-2 (TRBV11-2), which correlates with MIS-C severity and serum cytokine levels, consistent with a SAg-triggered immune response. Computational sequence analysis of SARS-CoV-2 spike further identified conserved neurotoxin-like motifs which may alter neuronal cell function and contribute to neurological symptoms in COVID-19 and MIS-C patients. Additionally, autoantibodies are detected during MIS-C, which may indicate development of post-SARS-CoV-2 autoreactive and autoimmune responses. Finally, prolonged persistence of SARS-CoV-2 RNA in the gut, increased gut permeability and elevated levels circulating of S1 have been observed in children with MIS-C. Accordingly, we hypothesize that continuous and prolonged exposure to the viral SAg-like and neurotoxin-like motifs in SARS-CoV-2 spike may promote autoim
Frontiers | Multisystem Inflammatory Syndrome in Children and Long COVID: The SARS-CoV-2 Viral Superantigen HypothesisMultisystem inflammatory syndrome in children (MIS-C) is a febrile pediatric inflammatory disease that may develop weeks after initial SARS-CoV-2 infection or exposure. MIS-C involves systemic hyperinflammation and multiorgan involvement, including severe cardiovascular, gastrointestinal (GI) and neurological symptoms. Some clinical attributes of MIS-C—such as persistent fever, rashes, conjunctivitis and oral mucosa changes (red fissured lips and strawberry tongue)—overlap with features of Kawasaki disease (KD). In addition, MIS-C shares striking clinical similarities with toxic shock syndrome (TSS), which is triggered by bacterial superantigens (SAgs). The remarkable similarities between MIS-C and TSS prompted a search for SAg-like structures in the SARS-CoV-2 virus and the discovery of a unique SAg-like motif highly similar to a Staphylococcal enterotoxin B (SEB) fragment in the SARS-CoV-2 spike 1 (S1) glycoprotein. Computational studies suggest that the SAg-like motif has a high affinity for binding T-cell receptors (TCRs) and MHC Class II proteins. Immunosequencing of peripheral blood samples from MIS-C patients revealed a profound expansion of TCR β variable gene 11-2 (TRBV11-2), which correlates with MIS-C severity and serum cytokine levels, consistent with a SAg-triggered immune response. Computational sequence analysis of SARS-CoV-2 spike further identified conserved neurotoxin-like motifs which may alter neuronal cell function and contribute to neurological symptoms in COVID-19 and MIS-C patients. Additionally, autoantibodies are detected during MIS-C, which may indicate development of post-SARS-CoV-2 autoreactive and autoimmune responses. Finally, prolonged persistence of SARS-CoV-2 RNA in the gut, increased gut permeability and elevated levels circulating of S1 have been observed in children with MIS-C. Accordingly, we hypothesize that continuous and prolonged exposure to the viral SAg-like and neurotoxin-like motifs in SARS-CoV-2 spike may promote autoim
Read more »
 Co-infection and ICU-acquired infection in COVID-19 ICU patients: a secondary analysis of the UNITE-COVID data set - Critical CareBackground The COVID-19 pandemic presented major challenges for critical care facilities worldwide. Infections which develop alongside or subsequent to viral pneumonitis are a challenge under sporadic and pandemic conditions; however, data have suggested that patterns of these differ between COVID-19 and other viral pneumonitides. This secondary analysis aimed to explore patterns of co-infection and intensive care unit-acquired infections (ICU-AI) and the relationship to use of corticosteroids in a large, international cohort of critically ill COVID-19 patients. Methods This is a multicenter, international, observational study, including adult patients with PCR-confirmed COVID-19 diagnosis admitted to ICUs at the peak of wave one of COVID-19 (February 15th to May 15th, 2020). Data collected included investigator-assessed co-infection at ICU admission, infection acquired in ICU, infection with multi-drug resistant organisms (MDRO) and antibiotic use. Frequencies were compared by Pearson’s Chi-squared and continuous variables by Mann–Whitney U test. Propensity score matching for variables associated with ICU-acquired infection was undertaken using R library MatchIT using the “full” matching method. Results Data were available from 4994 patients. Bacterial co-infection at admission was detected in 716 patients (14%), whilst 85% of patients received antibiotics at that stage. ICU-AI developed in 2715 (54%). The most common ICU-AI was bacterial pneumonia (44% of infections), whilst 9% of patients developed fungal pneumonia; 25% of infections involved MDRO. Patients developing infections in ICU had greater antimicrobial exposure than those without such infections. Incident density (ICU-AI per 1000 ICU days) was in considerable excess of reports from pre-pandemic surveillance. Corticosteroid use was heterogenous between ICUs. In univariate analysis, 58% of patients receiving corticosteroids and 43% of those not receiving steroids developed ICU-AI. Adjusting for potential c
Co-infection and ICU-acquired infection in COVID-19 ICU patients: a secondary analysis of the UNITE-COVID data set - Critical CareBackground The COVID-19 pandemic presented major challenges for critical care facilities worldwide. Infections which develop alongside or subsequent to viral pneumonitis are a challenge under sporadic and pandemic conditions; however, data have suggested that patterns of these differ between COVID-19 and other viral pneumonitides. This secondary analysis aimed to explore patterns of co-infection and intensive care unit-acquired infections (ICU-AI) and the relationship to use of corticosteroids in a large, international cohort of critically ill COVID-19 patients. Methods This is a multicenter, international, observational study, including adult patients with PCR-confirmed COVID-19 diagnosis admitted to ICUs at the peak of wave one of COVID-19 (February 15th to May 15th, 2020). Data collected included investigator-assessed co-infection at ICU admission, infection acquired in ICU, infection with multi-drug resistant organisms (MDRO) and antibiotic use. Frequencies were compared by Pearson’s Chi-squared and continuous variables by Mann–Whitney U test. Propensity score matching for variables associated with ICU-acquired infection was undertaken using R library MatchIT using the “full” matching method. Results Data were available from 4994 patients. Bacterial co-infection at admission was detected in 716 patients (14%), whilst 85% of patients received antibiotics at that stage. ICU-AI developed in 2715 (54%). The most common ICU-AI was bacterial pneumonia (44% of infections), whilst 9% of patients developed fungal pneumonia; 25% of infections involved MDRO. Patients developing infections in ICU had greater antimicrobial exposure than those without such infections. Incident density (ICU-AI per 1000 ICU days) was in considerable excess of reports from pre-pandemic surveillance. Corticosteroid use was heterogenous between ICUs. In univariate analysis, 58% of patients receiving corticosteroids and 43% of those not receiving steroids developed ICU-AI. Adjusting for potential c
Read more »
 Millisle: Thousands of people attend Ards Peninsula Kite FestivalThousands of people have attended a kite flying festival on the Ards Peninsula ⛅️ ANDborough
Millisle: Thousands of people attend Ards Peninsula Kite FestivalThousands of people have attended a kite flying festival on the Ards Peninsula ⛅️ ANDborough
Read more »
